India faces a global health crisis as the number of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections reaches over 23.7 million. As the country's health system buckles with increased admissions and a lack of resources, another health threat has emerged.
Public health officials report a rare black fungus infection, called mucormycosis, which is increasingly seen in vulnerable patients, including those with COVID-19 disease.
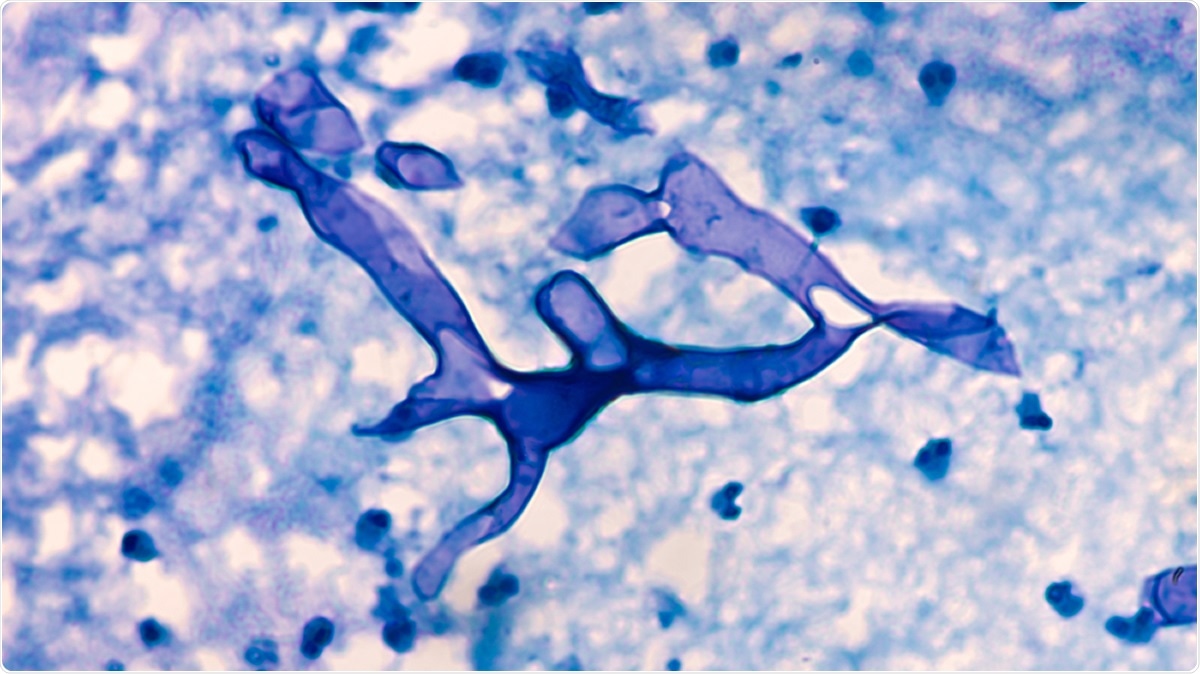
Mucormycosis: Broad, wide-angle non-septate hyphae of the fungus Mucor, from the paranasal sinus of a patient with diabetes mellitus. Image Credit: David A Litman / Shutterstock
What is mucormycosis?
Mucormycosis is a very serious and potentially fatal infection caused by exposure to mucor mold. Mucor is a microbial genus of approximately 40 species of molds commonly found in soil, plants, decaying fruits and vegetables, and manure.
The fungal infection commonly affects the sinuses of the lungs after inhaling fungal spores from the air. The fungi can also enter the skin after a cut, burn, or skin injury.
The mortality rate of this infection is about 50 percent. It impacts high-risk populations due to their reduced immune system function, including those with diabetes, cancer, and human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS).
Mucormycosis may cause symptoms like coughing out blood, blackening over the nose, blurred vision, chest pain, and breathing difficulties. A classic feature of this infection is tissue necrosis or tissue death. If the fungus spreads to the eyes, the patient may develop blurred vision, drooping eyelids, swelling, and possible vision loss.
The fungal infection is not contagious and does not spread between people and animals. There is no vaccine to prevent the infection.
India and the fungal infection
India sees an increase in mucormycosis cases, partly because many people grapple with SARS-CoV-2 infection. The COVID-19 pandemic created conditions for the infection to thrive and spread. The immune system of residents is compromised by SARS-CoV-2, allowing the black fungi to take hold.
The black fungus impacts the health of people with comorbidities, like diabetes and weakened immune systems. One of the ways COVID-19 is being treated is through high-dose steroids to treat inflammation. However, the drug can suppress the immune system, making it easier for other pathogens to take advantage.
As two infections continue to wreak havoc, India's health care system is on the brink of collapse.
In the western state of Maharashtra, including Mumbai, doctors report that around 200 patients who had recovered from COVID-19 were being treated for mucormycosis. Of these patients, eight died.
Meanwhile, in Gujarat, the local government ordered the allocation of separate wards in hospitals. Further, the officials ordered 5,000 doses of amphotericin B, the drug used to treat the fungal infection. New Delhi also reported cases of mucormycosis.
India has not released national data on the new infections but said there is no major outbreak.
Threat for diabetics
Mucormycosis may become potentially fatal in some individuals, including diabetics. The fungal infection is known to attack people who have compromised immune systems, especially those with diabetes.
People who have diabetes have weakened immune systems, making it easier for the fungi to cause infection. Apart from this, diabetics are at a higher risk of mucormycosis since the fungi love iron-rich, acidic environments, and diabetic ketoacidosis, a condition in diabetics that causes the blood to become acidic.
How to prevent mucormycosis infection?
Due to its increased fatality rate, people should be proactive in protecting themselves. They should avoid areas with dust, including excavation and construction sites. Avoid contact with water-damaged buildings and floodwater and prevent joining activities that involve close contact with soil and dust. When handling soil, make sure to use protective gloves and wash the hands with soap and water.
In treating fungal infection, patients need to receive treatment promptly. Usually, antifungal drugs will be given to kill the fungi.